Table of Contents
What is Psoriasis?
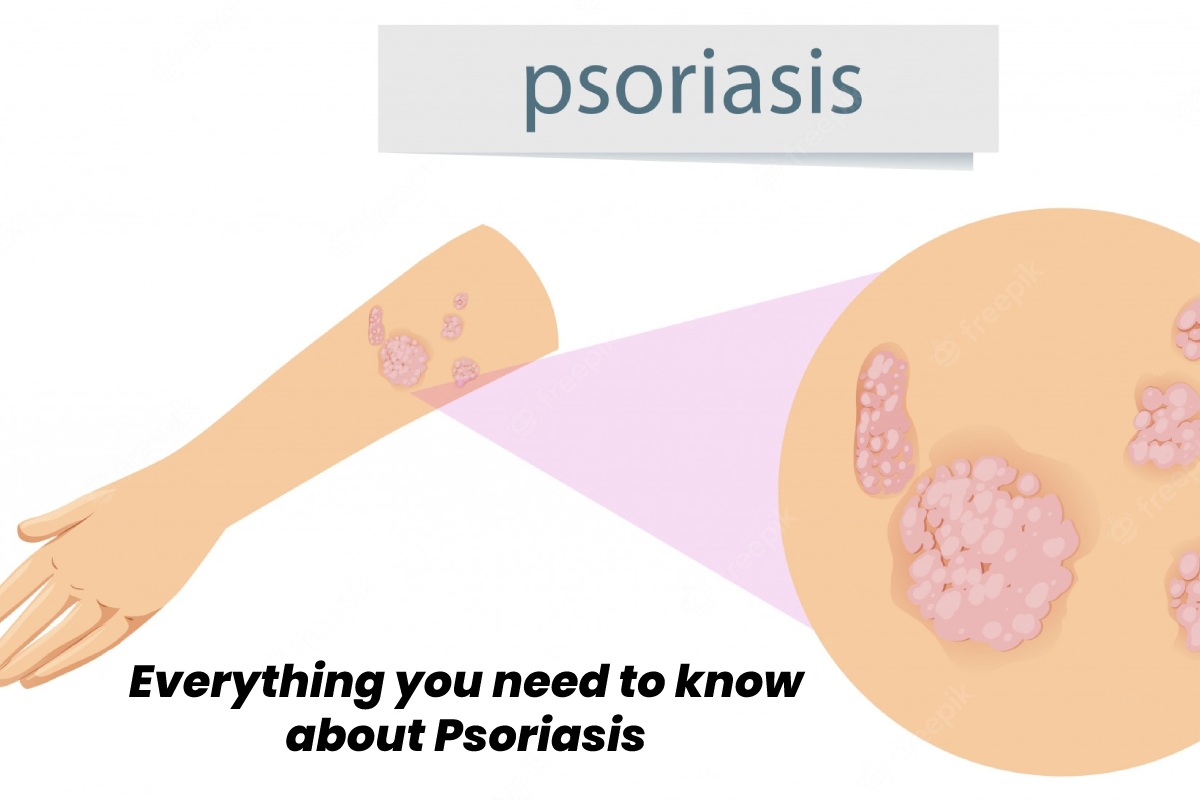
Psoriasis is a chronic autoimmune disease that sources the rapid buildup of skin cells. This buildup of cells causes flaking on the surface of your skin.
Typical psoriatic scales are whitish and develop into thick, red patches. However, on darker skin tones, they may also appear more purplish, dark brown with scales of grey. Inflammation and redness around the scales are pretty joint. Sometimes these patches crack and bleed.
Psoriasis is the result of an accelerated process of skin production. Typically, skin cells grow deep into your skin and slowly rise to the surface. Eventually, they fall. The distinctive life cycle of a skin cell is one month.
The production process can occur in people with Psoriasis in just a few days. Due to this, the skin cells do not have time to fall off. The rapid overproduction leads to the buildup of skin cells.
The scales usually grow on the joints, such as the elbows and knees. However, they can develop anywhere on your body, including:
hands
feet
neck
scalp
Face
Less common types of psoriasis affect:
nails
stuffy
the area around the genitals
According to a study in 2021, approximately 7.5 million American adults aged 20 and older have Psoriasis – a prevalence rate of 3% (disease onset). By race and culture, the prevalence rates are:
3.6% white
3.1% of non-Hispanic people, including multiracial people
2.5% of Asians
1.9% of Hispanics, including Mexican Americans
1.5% of blacks
It is usually associated with several other conditions, including:
Type 2 diabetes
inflammatory bowel disease
psoriatic arthritis
anxiety
Depression
What are the Types of Psoriasis?
There are five kinds of Psoriasis:
Plaque Psoriasis
Plaque psoriasis is the most mutual type of Psoriasis.
American Academy of Dermatology (AAD) estimates that approximately 80-90% of people with this condition have plaque psoriasis. It causes red, inflamed patches on fair skin and purple, greyish, or dark brown patches on coloured skin, making it difficult to diagnose in people of colour.
These patches are often covered with silvery whitish scales or patches and are often more pronounced on coloured skin. Although, These plaques are commonly found on the elbows, knees, and scalp.
Guttate Psoriasis
Guttate Psoriasis usually occurs in childhood. And also, This type of Psoriasis causes small pink or purple patches. These patches are rarely thick or raised, as in plaque psoriasis. The most common areas of guttate Psoriasis are the trunk, arms, and legs.
Pustular Psoriasis
Pustular Psoriasis is more common in adults. This causes white, pus-filled blisters, large red or purple patches, and inflamed skin depending on skin tone. It can look like a more intense purple colour on darker skin tones. Pustular Psoriasis is usually localized to small areas of the body, such as the arms or legs, but can be widespread.
Reverse Psoriasis
Inverse Psoriasis causes clear patches of red, shiny, inflamed skin. Reverse patches of Psoriasis develop under the arms or chest, in the groin, or around skin folds on the genitals.
Erythrodermic Psoriasis
According to the National Psoriasis Foundation, erythrodermic Psoriasis is a severe and rare type of Psoriasis.
This shape often covers large parts of your body at the same time. As a result, the skin looks almost tanned. In addition, the developing scales often break off in large patches or sheets. It is not uncommon for you to develop a fever or become seriously ill with this form of Psoriasis.
Psoriasis is an autoimmune disease. Autoimmune diseases are the result of your body attacking itself. In Psoriasis, white blood cells called T-lymphocytes mistakenly attack your skin cells.
Generally, white blood cells in the body are used to attack and destroy invading bacteria and create a defence against infection. However, this erroneous autoimmune attack leads to an acceleration in the production of skin cells. Accelerated production of skin cells leads to the too rapid growth of new skin cells. As a result, they are pushed to the skin’s surface, where they accumulate.
This leads to the plaques that are most commonly associated with Psoriasis. Attacks on skin cells also cause red, inflamed patches of skin to appear.
Genetic
Some people inherit genes that make them extra likely to develop Psoriasis. In addition, a close relative with this skin condition is at an increased risk of developing Psoriasis, according to a study published in 2019.
Learn more about the causes of Psoriasis.
Diagnose Psoriasis
Two tests or examinations may be required to diagnose Psoriasis.
Physical examination
Maximum doctors can make a diagnosis with a simple physical examination. The symptoms of Psoriasis are usually evident and easily distinguished from other conditions that can cause similar symptoms.
During this checkup, be sure to show your doctor anything that is bothering you. Also, tell your doctor if any of your family members have a medical condition.
Biopsy
If your symptoms are unclear or your doctor wants to confirm a suspected diagnosis, they may take a small sample of your skin. This is called a biopsy.
A biopsy can be done in the doctor’s office on the day of the appointment. Your doctor will likely inject a local anaesthetic to make the biopsy less painful.
They will send the skin biopsy to a lab for analysis, where it will be examined under a microscope. An examination can diagnose the type of [Psoriasis] you have. It can also rule out other possible illnesses or infections.
When the results come back, your doctor may schedule an appointment to discuss the results and treatment options.
Psoriasis Triggers
[Psoriasis] triggers: stress, alcohol, etc.
External “triggers” can provoke a new attack of [Psoriasis]. And also, these triggers are not the same for everyone. Although, they may also change over time for you.
The most common triggers for [Psoriasis] include:
Stress
Unusually severe stress can trigger an exacerbation. However, if you learn how to reduce and manage stress, you can reduce and possibly prevent flare-ups.
Alcohol
An alcohol use disorder can exacerbate [Psoriasis]. If you drink excessively, [psoriasis] flares may be more frequent. Reducing alcohol or quitting smoking isn’t just good for the skin. Your doctor can help devise a plan for dealing with your drinking problems if you need help.
Hurt
An accident, cut, or scratch can trigger an aggravation. Injections, vaccines, and sunburns can trigger a new epidemic.
Medications
Some medications are considered triggers for Psoriasis. These drugs include:
lithium
antimalarial drugs
blood pressure medicine
Infection
[Psoriasis] is caused, by the immune system mistakenly assaultive healthy skin cells. If you are sick – perhaps you have an infection – your immune system may incorrectly mount an immune response against itself in addition to protecting itself against the infection.
This can trigger a new outbreak of Psoriasis. Strep throat is a common trigger.
Here are ten other psoriasis triggers you can avoid.
Treatment options for Psoriasis
[Psoriasis] is incurable. Treatment is aimed at:
reduce inflammation and flaking
, slow down the growth of skin cells,
remove the plates
Treatment for Psoriasis falls into three categories:
Local Treatment
Creams applied directly to the skin can help reduce mild to moderate Psoriasis/
Topical treatments for [Psoriasis] include:
topical corticosteroids
anthralin
vitamin D analogues
salicylic acid
moisturizing cream
Systemic Drugs
People with moderate to severe [psoriasis] and those who have not responded to other treatments may need to use oral or injectable medications.
Many of these drugs can have serious side effects, so doctors usually prescribe them for a short period.
These drugs include:
methotrexate
cyclosporine (Sandimmun)
organic products
oral retinoids
Light Therapy
This [psoriasis] treatment uses ultraviolet (UV) light or natural light. Sunlight kills overactive white blood cells, which attack healthy skin cells and cause cells to proliferate. UVA and UVB rays can help reduce mild to moderate psoriasis symptoms.
Most people with moderate to severe psoriasis will benefit from a combination of treatments. This type of therapy uses more than one treatment to reduce symptoms. Some people may use the same treatment all their lives. Others may need to change treatments from time to time if their skin stops responding to the treatment they receive.